For patients with chronic lung disease and hypoxemia complications, oxygen use has been extended from inpatient to outpatient care. This article introduces the general situation of oxygen devices (oxygen concentrator, compressed gas cylinders and liquid oxygen) and delivery systems (high and low flow rate) . The indications, advantages and disadvantages of each device and transmission system are described. The appropriate device and transmission system can be selected according to the needs of each patient.
For patients with chronic lung disease and hypoxemia complications, the following three groups of patients with chronic hypoxemia lung disease are suitable for long-term oxygen therapy (LTOT) :
1. Patients with arterial oxygen tension (PaO2) ≤55 mmHg at rest in nonrecumbent position, despite optimal treatment of underlying condition.
2. Patients with PaO2 >55 mmHg associated with evidence of central nervous system dysfunction, cor pulmonale, secondary pulmonary hypertension or polycythaemia.
3. Patients with demonstrable fall in PaO2 below 55 mmHg and desaturation during sleep and/or exercise.
LTOT use is now higher among women and is expected to increase further in the near future due to the high number of middle-aged female smokers. There are a variety of oxygen-saving devices available, and given the high cost of LTOT and its impact on patients’health-related quality of life, the choice and prescription of the best devices requires a clear understanding of these devices in the following paragraphs, we will introduce different oxygen devices and delivery systems.
Oxygen concentrators
How do they work?
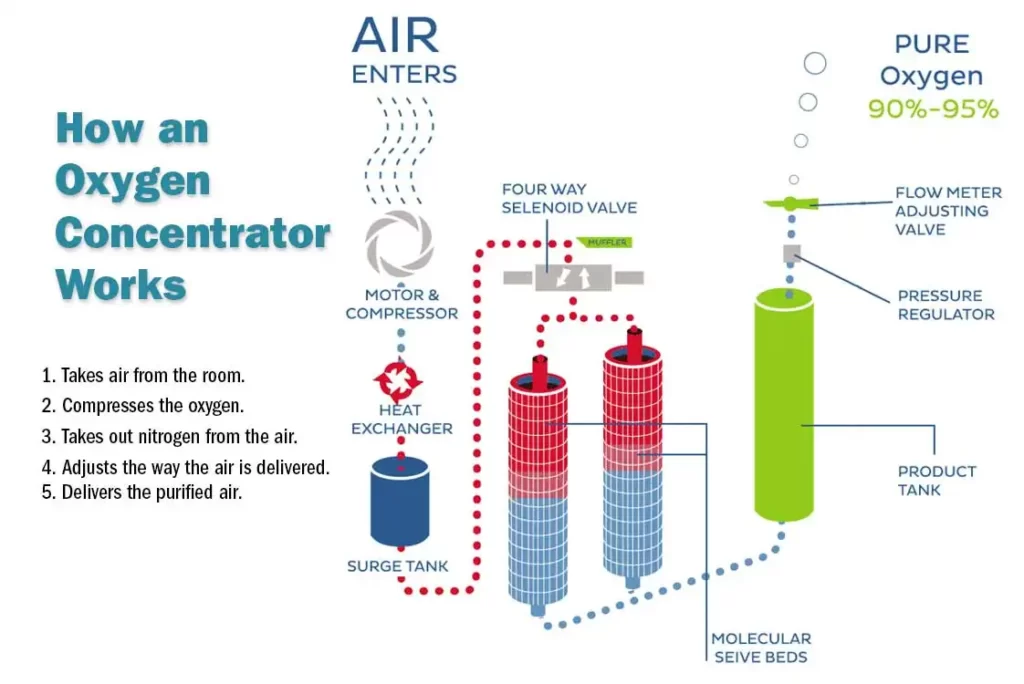
Oxygen concentrators provide a safe source of oxygen-rich air.
An oxygen concentrator (sometimes called an oxygen generator) is a device that draws indoor air through a series of filters that remove dust, bacteria, and other particles. In the first stage of the concentration process, the machine forces air into one of two cylinders containing a molecular sieve material or a semi-permeable membrane, in which nitrogen is absorbed, this leaves concentrated oxygen (90% or more) and a small fraction of other gases in the indoor air.
At the same time, in another cylinder, nitrogen is desorbed and drawn into the atmosphere. In the second step, the cylinder’s function is reversed in a timed cycle, providing the patient with a continuous flow of oxygen. A typical oxygen concentrator can provide 0.5-5 l/min of oxygen flow (low flow oxygen concentrator) , while some models can provide up to 10 l/min of oxygen flow (high flow oxygen concentrator) .
Types of oxygen concentrators and oxygen delivery
There are two types of oxygen concentrators: stationary and portable.
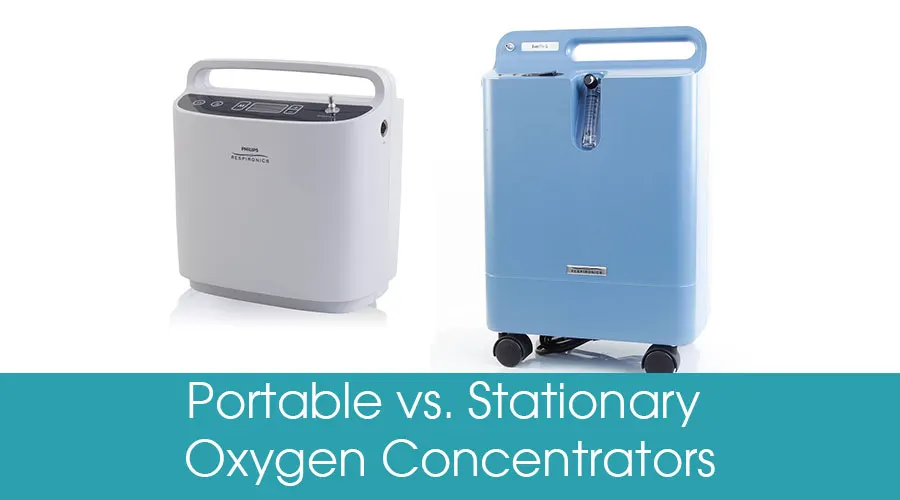
Stationary (domestic) concentrators provide an uninterrupted supply of oxygen with a flow rate in the range of 0.5-15 L/min. Their average weight is about 10 kilograms. They have several ergonomic handles built in, offering the option of lifting or rolling the device. New miniature concentrators, making stationary concentrators more mobile than ever. The concentrator plugs into the main power supply at home and uses 300 watts (or less) per hour (about the equivalent of four light bulbs) . Backup compressed gas cylinders are sometimes provided for use in the event of a power failure.
A relatively new option is an ultra-small home oxygen concentrator that can weigh about 4.5 kg. These devices can use either alternating current (AC; e. g. from a wall outlet) or direct current (DC; E. G. from a lighter outlet) , and they can move (for example, they can easily move from room to room, or they can be transported by car) . They currently support oxygen flow up to 2 L/min.
Portable oxygen concentrators are the latest technology for LTOT users, who want small, lightweight and portable oxygen solutions in a compact and mobile unit. Portable concentrator weight, size, oxygen flow setting, range of 1L/min and battery life, and other specifications.
The main differences between stationary and portable concentrators can be summarized into four main factors:
- oxygen output
- volume and weight
- power selection
- Price
- Stationary oxygen concentrators have higher oxygen output and lower cost.
- Portable oxygen concentrators are smaller, lighter, and have greater flexibility and power.
- Portable oxygen concentrators are the best option for patients who are active and often away from AC (wall outlet) power. Most portable oxygen concentrators use lithium-ion battery, which degrades over time. Most of these batteries can be recharged about 300 times without significant degradation.
In general, there are two types of oxygen transfer in oxygen concentrators: continuous flow dose transfer and pulse mode transfer. The continuous flow dose delivery provides a stable and reliable oxygen flow based on the L/min setting, while the pulse mode delivery provides a pulsatile oxygen “bolus” when the user begins to breathe. Initially, you should adjust your individual traffic settings.
Indications
Stationary oxygen concentrators are often used by LTOT patients because they are cost-effective and safer than compressed gas cylinders. Oxygen concentrators are recommended for patients who use oxygen for more than 1.4 hours per day. The guidelines do not give instructions for choosing a transport device, but only recommend portable devices for frequent LTOT patients.
Portable oxygen concentrators for outpatient oxygen therapy are available to people already in the LTOT who want to use oxygen outside the home. Dynamic oxygen therapy can improve exercise endurance and breathing difficulties, although for most chronic obstructive pulmonary disease, oxygen before and after exercise is not beneficial. In addition, outpatient oxygen therapy can increase daily oxygen use and/or better compliance.
Advantages and disadvantages
| Advantages | 1. The proper use of an oxygen concentrator can improve the survival rate of respiratory diseases, improve psychological attention, enhance endurance and improve mood. 2. In patients with chronic obstructive pulmonary disease, the duration of the oxygen supply itself affects survival. In chronic obstructive pulmonary disease of hypoxemia, mortality was lower with continuous oxygen therapy than with nocturnal oxygen therapy. 3. The oxygen concentrator does not need to be refilled and can provide an unlimited amount of oxygen. 4. In the long run, concentrators are more cost-effective than compressed gas cylinders and can last up to 15,000 hours. |
| Disadvantages | 1. Oxygen concentrators need electricity to work properly, and it is necessary to install a backup generator at home in case of a power failure. 2. Patients using stationary oxygen concentrators need to consider weekly filter changes, regular maintenance, and warm-up periods for the machine. 3. Some of the equipment is loud and vibrating. |
Related costs
The global market value of medical oxygen concentrators was $1.75 billion in 2018. Between 2019 and 2025, the market is expected to expand at a compound annual growth rate of 7.4 percent. The price of the new home oxygen concentrator, which ranges from $595 to $2,000, depends on batteries and other accessories. Used oxygen concentrators are cheaper ($595-$1500) , depending on the time, warranty and equipment. However, the rental of stationary oxygen concentrators can be increased from $35 per day to more than $200 per week, with a discount for an extension of the lease. In the recent two years, with the appearance of Covid-19, increased the intense demand for oxygen-making machines, so that the price of oxygen-making machines doubled.
Compressed gas cylinders
Differences between oxygen concentrators and compressed gas cylinders:

| Item | Oxygen concentrators | Compressed oxygen cylinders |
| Power source required | Yes, continuously (according to model: 100–600 W) | No |
| Transport required | Only at the time of installation | Yes, regularly; heavy and costly to transport |
| Exhaustible oxygen supply | No, continuous supply as long as power remains uninterrupted | Yes, depending on the size, storage pressure, and patient needs |
| User care | Moderate: cleaning of filters and device exterior, and minimise fire hazard | Minimal: regular checking, minimise fire hazard (no grease or flammables) |
| Operational costs | Small: electricity and maintenance | High: cylinder refills and transport from refilling station to a hospital |
| Maintenance | Moderate: check for low oxygen output with an analyser | Moderate: check for pressure leaks with gauge |
Properties, classification and appearance
A cylinder is a metal container filled with compressed gas and held under high pressure. The oxygen capacity is determined by the size range of the oxygen cylinder. For compressed oxygen cylinders, there are three ways to transport portable oxygen:
- Portable oxygen cylinders
- Light oxygen cylinders
- Domestic oxygen cylinders
When filled with oxygen, cylinders range from small portable portable walking-use cylinders (such as 53 cm tall, 3 kg in weight, and 430 litres of oxygen) to large static cylinders (such as 71 cm tall, 18 kg in weight, and 2,122 litres of oxygen) . Depending on the patient’s level of activity and fitness, exercise may require a knapsack, handcart, or wheeled handcart, depending on cylinder size and weight. Oxygen cylinders are marked in white to distinguish them from other medical gases.
How do they work?
A regulator is attached to the top of the cylinder and operates like a faucet, allowing for safe adjustment of oxygen flow, in L/min units. When the faucet is turned on manually, oxygen is delivered to the patient’s body where resistance is least by means of an oxygen delivery device, such as one with a mask or nasal cannula. The pressure reading (barometer) shows the remaining oxygen pressure in the cylinder to estimate the amount of oxygen available.
The capacity of the compressed oxygen tank is relatively low: for example, at 200 bar of air pressure and 400 litres of oxygen, the patient will have enough oxygen to last 2.5 hours, depending on the flow rate.
At home or in hospitals, cylinders are replaced by gas suppliers. The frequency of delivery depends on the cylinder size and oxygen consumption. A home-filled cylinder can be refilled with an oxygen concentrator.
In contrast to continuous oxygen flow, oxygen-saving devices provide pulse oxygen only when a patient inhales. These “on demand” oxygen delivery systems enable cylinders to last longer because less oxygen is wasted during exhalation. Studies have shown that health services can reduce oxygen use by 50%, thus reducing the number of home births and thus the cost. However, oxygen retention devices vary in their ability to maintain arterial oxygen saturation levels during exercise, and some patients have difficulty triggering these devices due to advanced lung disease.
Indications
Compressed gas cylinders are usually used in conjunction with an oxygen concentrator for patients who require supplemental oxygen at home. These patients are immobile, spend most of their time at home, and require little portable oxygen, which is why compressed gas cylinders can be used as a backup in the event of a power failure or concentrator failure.
In hospitals, mobile compressed gas cylinders are primarily used to provide temporary oxygen to patients undergoing invasive ventilation that requires diagnostic or therapeutic procedures outside the intensive-care unit.
Correlation with clinical outcomes
When standard portable cylinders were compared with lightweight cylinders in patients with COPD, in a prospective, randomised, clinical, multicentre trial conducted by the COPD Clinical Research Network, no differences were found in activity levels, oxygen saturation, Borg score or 6-min walk test.
Advantages and disadvantages
| Advantages | Cylinders combined with a stationary oxygen concentrator provide a more permanent oxygen supply. |
| Disadvantages | Cylinders are less portable than oxygen concentrators. The oxygen supply is less than that of liquid oxygen, and the outdoor activity time is obviously shortened. |
Liquid oxygen
The introduction of liquid oxygen has changed the landscape of home oxygen therapy. The first domestic LOX system was developed in 1965 to provide a larger stationary oxygen system at home, using smaller portable LOX devices that can be filled and used outside the home.

How do liquid oxygen systems deliver oxygen?
Liquid oxygen is a cryogenic liquid, i. e. a liquefied gas with a boiling point of-183 ° C.
Liquid oxygen allows a larger amount of oxygen (gas) to be stored as a liquid in a small container. The 860:1 expansion of liquid oxygen means that when a liter of liquid oxygen evaporates, it expands to about 860 liters of gaseous oxygen.
Liquid oxygen for medical use (at least 99.5% pure) must first be vaporized into a compressed gas and then heated at room temperature in the device before the patient can deliver oxygen through a tube through the nose to the nostrils. How long a patient can stay in a portable flask depends on the rate of oxygen flow that the patient is using, as prescribed by the treating physician.
Fixed storage containers (“parent containers”) and portable containers have different sizes.
These cryogenic vessels keep the liquid at a low temperature. Small fixed containers can provide a convenient supplemental supply in a car or truck during a long trip from home. If the patient is using high-flow liquid oxygen (up to 15 L/Min continuous flow of oxygen) , it is important to note that ice may form on the portable heat exchange coil due to ambient humidity freezing. These patients usually have two portable systems to facilitate continuous use, allowing deicing in one unit while using portable oxygen in the other.
Indications
Choosing the right oxygen delivery system for the right candidate is a challenge for clinicians. The choice of liquid oxygen and oxygen in compressed gas cylinders is determined by two main factors, namely, convenience and efficiency. For outpatient patients who wish to move, limited French data from the ANTADIR registry support the use of portable liquid oxygen for this group of patients. According to the literature, liquid oxygen may be suitable for those who are able to return to work, require a flow rate greater than 5 L/Min, and are able to walk, a chronic respiratory disorder patient who is unable to move without an oxygen supply. Liquid oxygen is the most practical option for outpatients who require high-flow oxygen. Figure 3 shows a patient with a nasal cannula and a liquid oxygen tank.
Correlation with clinical outcomes
Patients who used liquid oxygen were more likely to stay out of the house and use daily oxygen for longer periods than patients who used oxygen concentrators. In addition, LOX treatment improves patient compliance and health-related quality of life. Significant differences were found in the following quality of life indicators for LOX therapy and oxygen concentrators: physical function, physical care, walking, social interaction, and disease impact scores.
Advantages and disadvantages
| Advantages | 1. Liquid oxygen occupies less space than gaseous oxygen and is more convenient and light to carry. Modern liquid oxygen tanks weigh 3.5 kg when full, 2.5 kg when empty, and are lighter for larger portable tanks. 2. Liquid oxygen tanks are safer than compressed gas cylinders because they have lower pressure.The increased availability of liquid oxygen is beneficial for chronic respiratory disease patients, who would otherwise receive only two hours of oxygen at most, thus limiting their outdoor activities and independence. 3. Liquid oxygen systems last longer and are easier to tank. |
| Disadvantages | 1. Oxygen tanks and liquid oxygen tanks have limited capacity. 2. The repeated delivery of oxygen increases costs. 3. Liquid oxygen continues to evaporate, requiring professional service providers to use and re-supply it at least two or three times a month, adding to costs. 4. Liquid oxygen can not be used on commercial aircraft. |
Oxygen delivery systems
Oxygen delivery system is divided into low flow system and high flow system. The low flow system provides lower oxygen flow than the actual inspiratory flow (~ 30L/Min) . As the patient breathes in, the oxygen is diluted by the indoor air, the degree of dilution depending on the inspiratory flow. As a result, these oxygen delivery systems do not allow for accurate calculation of inspiratory oxygen fraction (FIO2) . The high-flow oxygen delivery system provides a high oxygen flow rate, and the FIO2 is stable and unaffected by the patient’s breathing pattern.
Conclusions
The proper choice of oxygen devices and delivery systems depends on the degree of hypoxemia, the available evidence for the patient’s basic diagnosis, and the patient’s preferences. Respiratory physicians should have a unified knowledge of all devices and systems to design appropriate and individualized patient-based oxygen therapy plans.




2 Responses
Hi Claire, hope you are well. I am with a company xxx and am looking at supplying Oxygen to the home market. We will be filling cylinders from a PSA 93% and would like to offer oxygen concentrator . Do you have a representative in xxx?
Yes, we have. 1-50L/min oxygen flow rate, high purity, stable and reliable system, long working life, easy installation, low energy consumption.